Caregiver-Provider Disconnect: Why It Happens and How to Fix It
When communication breaks down between healthcare providers and family caregivers, everyone loses, especially the person living with a mental illness. In today’s blog, we’ll talk through why this breakdown happens and what caregivers and providers can do to build stronger relationships and foster healthy patterns of communication.
Introduction
Caregivers often see what providers can’t: changes in mood, missed meds, early signs of crisis. But too often, they’re left out of the conversation. On the other side of the equation, providers want to help but are constrained by time, privacy laws, and overloaded systems. Misunderstandings, especially around HIPAA, make everything harder.
The good news? There’s a better way. With a clearer understanding of what’s allowed and a few simple changes in how we share information, doctors and families can become true partners in care.
Why the Disconnect Happens
The relationship between caregivers and providers can be tricky. Caregivers are closely involved in their loved one’s day-to-day life, but they’re not the patient, which means they often can’t be part of medical conversations. Privacy rules can make it hard to get information, even when they’re trying to help. Providers only see the patient for short visits and may not know what’s really going on at home. Both care deeply, but they see different parts of the picture. That’s why working together is so important.
Before we dive into some tips that can improve communication, it helps to understand what’s getting in the way. Here are some common reasons why providers and caregivers struggle to connect and why these issues matter.
Privacy Laws (And Misunderstandings About HIPAA)
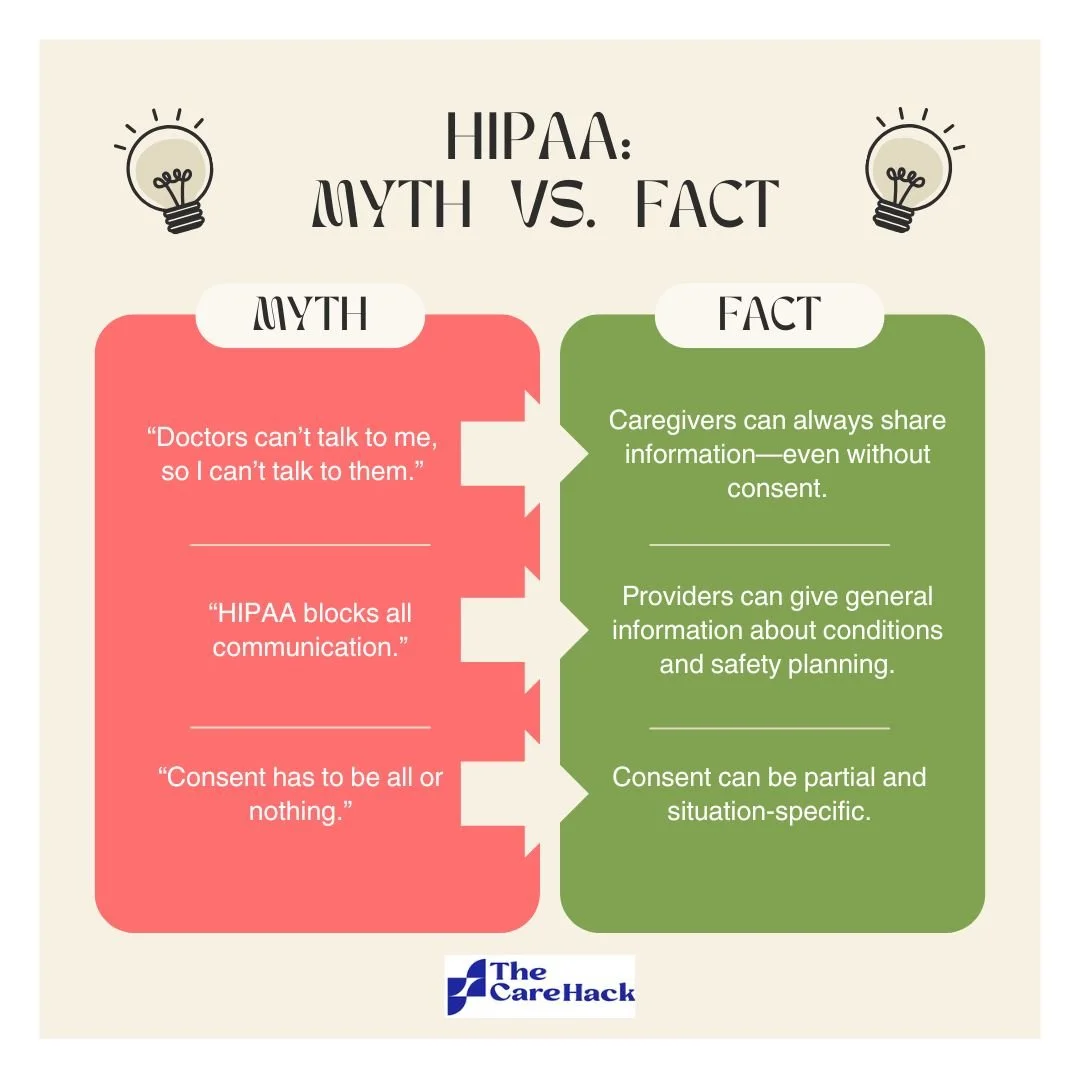
HIPAA is a federal law that protects a person’s private health information. One of its key components is that providers cannot share a patient’s medical details without their permission (unless the patient is in a life threatening emergency). In mental health care, this can easily get complicated, especially when someone is unsure about what is being asked or unwilling to give consent.
HIPAA protection is critical, but it’s often misinterpreted as a wall between providers and families. In reality, HIPAA allows more communication than most people realize.
When caregivers don’t have permission to access medical information, it can be hard to stay involved or support treatment. Providers often feel stuck. They want to include caregivers, but they are also legally required to protect their patient’s privacy.
What many people don’t know is that HIPAA doesn’t stop caregivers from sharing information with doctors. Even if a providers can’t speak openly with you, they can still listen to what you have to say. This is often overlooked during appointments, but it’s a key way you can stay involved and helpful, even without full access.
Different Perspectives
Caregivers live the day-to-day reality of mental illness beside their loved ones. They focus on behavior, safety, and daily support. Providers focus on clinical diagnoses, treatment adherence, and medical risk. Both perspectives are important, but they don’t always match up.
It’s normal for these differences to lead to frustration. When caregivers and providers struggle to understand each other, it can cause tension or disagreements about the best approach to care. And it’s never easy to convince someone to see things exactly the way you do.
That’s why it helps to think of the relationship as a team effort. You may see things differently, but you're working toward the same goal. When caregivers and providers combine their knowledge and experience, those different viewpoints can actually become a strength instead of a barrier.
Communication Channels Are Outdated Or Insecure
Clear and consistent communication between caregivers and providers is essential. But today, many of the tools caregivers and providers rely on—like phone calls or email—are outdated and not secure. These methods aren’t HIPAA-compliant, meaning they’re not safe for sharing private health information.
This communication gap creates real problems. Without a secure way to stay in touch, important updates from caregivers may be missed, and providers may struggle to get a full picture of what’s happening between appointments. It becomes harder to collaborate, coordinate care, and respond quickly when concerns arise.
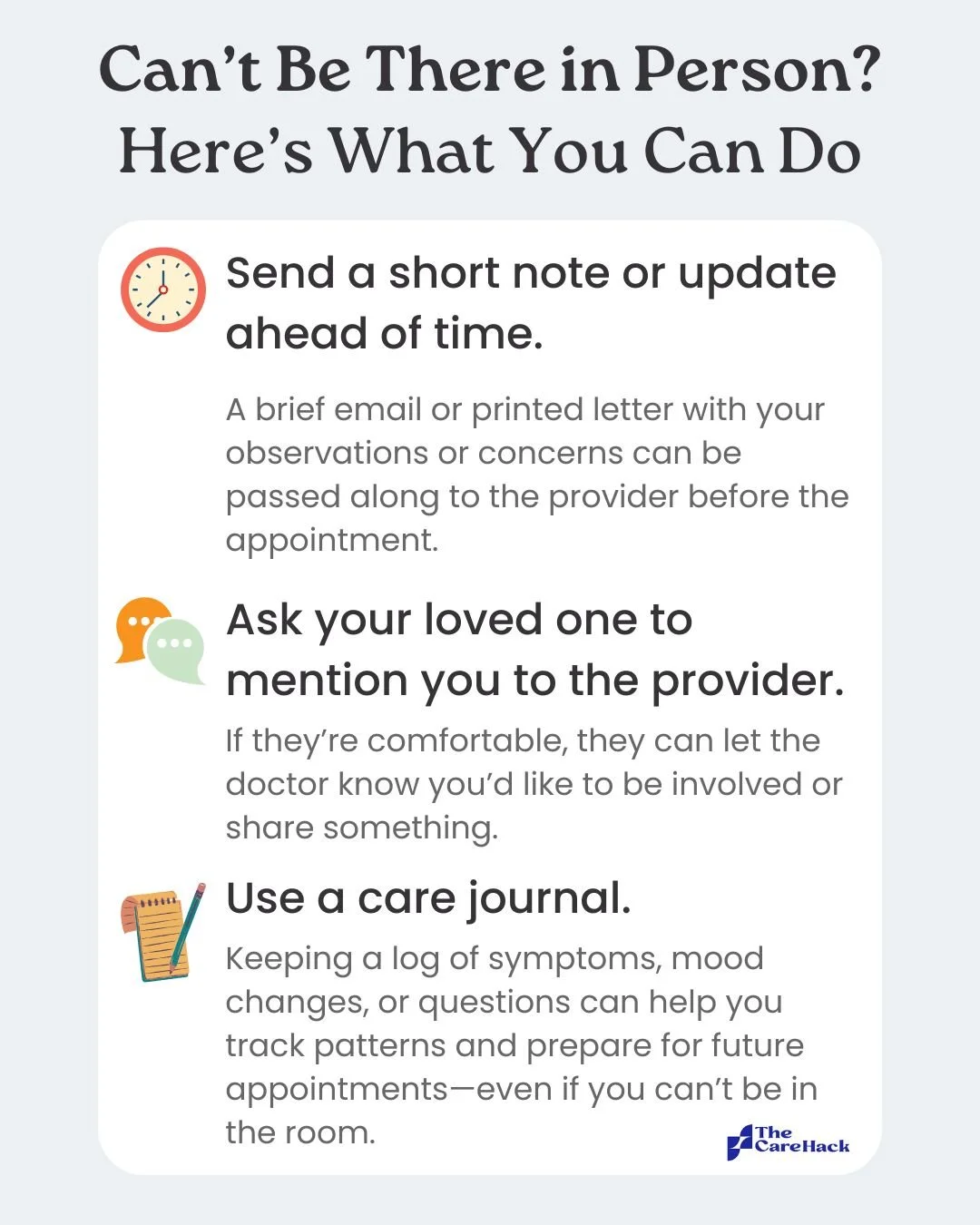
While in-person visits can offer the best chance for meaningful caregiver-provider communication, they’re not always possible. A lack of secure communication tools can add unnecessary stress to both caregivers and providers, especially in mental health settings where trust, timing, and context are key.
Time Constraints
Providers are overwhelmed. Appointments are short. There’s rarely time to hear from caregivers, especially if they’re not the patient. And caregivers may not know how to share what matters most.
That limited time makes every interaction count. Without clear systems or guidance for sharing important updates, key details can fall through the cracks, leaving both caregivers and providers feeling unheard and unsupported.
How Caregivers and Providers Can Build Stronger Communication
For Caregivers: How To Be Heard Without Overstepping
1. Be Physically Present Whenever You Can
Face-to-face conversations are the most direct and secure way for caregivers and providers to connect. When you go with your loved one to their doctor’s appointment, you're not just showing up for them. You’re also showing your provider that you want to be part of the care team. Including all three parties in these conversations helps build trust. It gives your loved one a chance to hear what’s being shared firsthand, reduces misunderstandings, and makes the whole process feel more transparent and respectful for everyone involved.
Being there in person also makes it easier to navigate privacy rules. In the clinic, a provider can simply ask, “Is it okay if your mom joins us today?” This kind of gentle, in-the-moment request is often more comfortable for someone with mental illness, compared to signing detailed forms or paperwork. They're also more likely to say yes when the ask feels casual and supportive.
These small, real-time moments can make a big difference. In-person visits help providers hear your voice, understand your perspective, and work with you, especially when time is short and communication is limited.
2. Think Of HIPAA As A One-Way Window
HIPAA can feel like a closed door, but it’s more like a one-way window. You can see in and share what’s happening on your side, even if nothing comes back through. Providers can’t always speak freely, but they can always listen to everything you share.
Use that to your advantage. You see your loved one every day. You notice the changes, the warning signs, and the subtle shifts that may not show up in a short appointment. Even if your loved one hasn’t given the provider permission to talk with you, you can still speak up.
Share clear, specific observations. For example: “He’s been sleeping 2 hours a night and pacing constantly for the last 3 days.”
This kind of detail gives providers essential context and helps guide better care. Your insight matters, even if they can’t respond directly. You’re part of the picture, and what you share can make a real difference.
3. Keep A Short And Strategic Notes Log
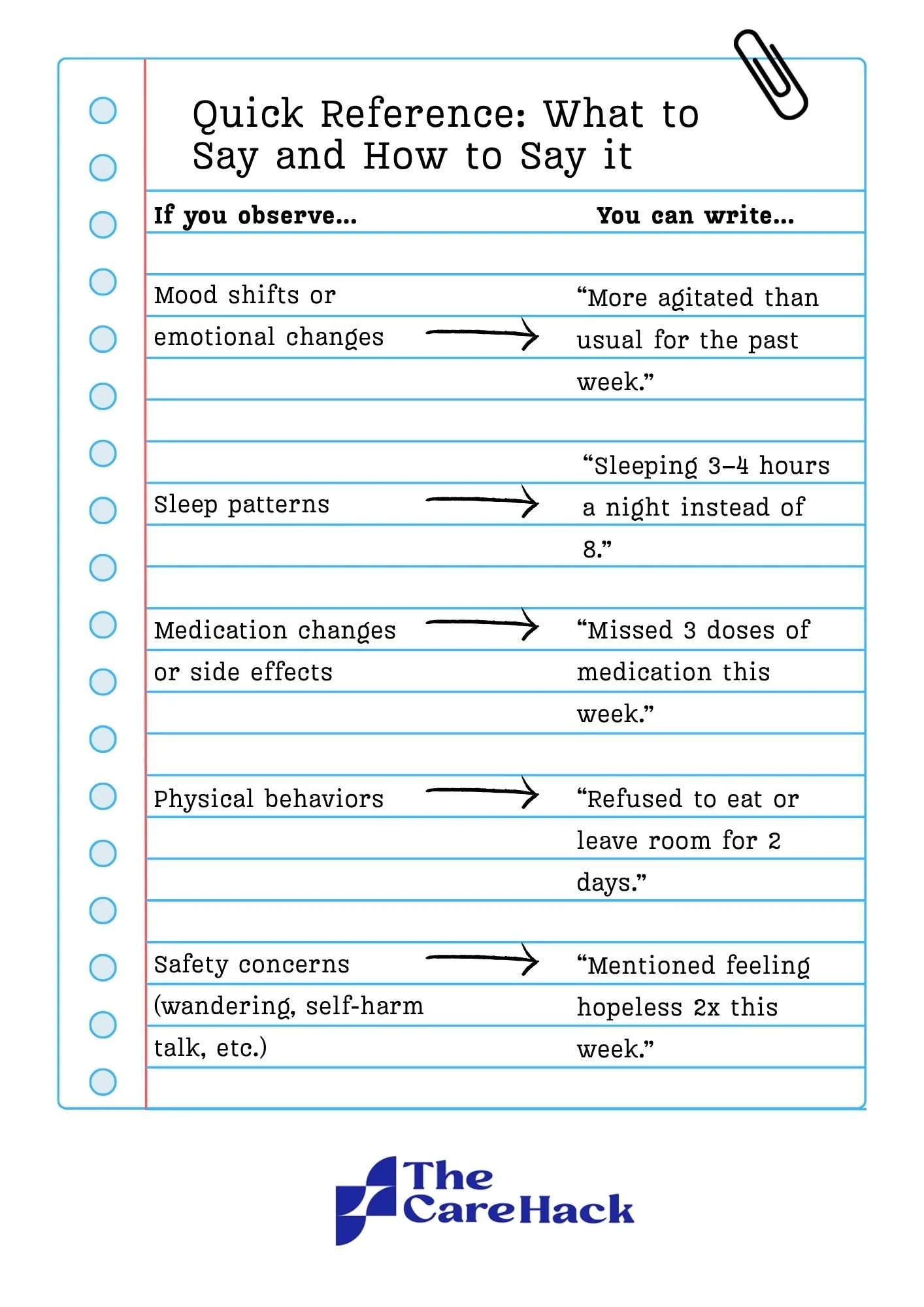
In a short doctor’s visit, it can be hard to remember everything and prioritize what’s most important to share. That’s where keeping a log can help.
Jot down changes in mood, sleep, behavior, or medication as they happen. The goal isn’t to write a long story—it’s to create a clear, useful snapshot of what’s going on. Stick to the facts, focus on patterns, and highlight any turning points.
A written log helps you come prepared to appointments. It also makes it easier for providers to quickly understand what you’re seeing at home. Your notes can be handwritten on paper, typed in bullet points on your phone, or, if you have extra time, organized in a document on your computer. As long as it’s easily accessible during your appointment, take notes in whichever way works best for you. Here are some signs and symptoms to take note of at home:
5. Speak As A Team Member
As a caregiver, you make up a core part of the care team. When you approach conversations with providers from that perspective, it helps build trust and collaboration.
One simple but powerful shift is to use “we” statements. Instead of saying, “I think the meds aren’t working,” try:
“We’ve noticed he’s been more withdrawn this week, and we’re hoping to figure out what might help together.”
Framing your thoughts this way shows that you’re not there to criticize—you’re there in partnership with the medical team. You and the provider both want what’s best for your loved one. When that shared goal is front and center, conversations become more productive, respectful, and focused.
6. Learn As You Go
Learning a little about your loved one’s condition or treatment plan can go a long way. Knowing the basics helps you understand what providers are saying and makes your questions more focused and helpful. When you’re informed, it’s easier to spot changes, understand treatment options, and speak up with confidence. A bit of background knowledge turns confusion into clarity, and it makes you an even stronger part of the care team.
Start small: read about the diagnosis, learn what the medications do, or ask the provider for a resource they trust. The more you know, the better prepared you’ll be.
For Providers: How to Create a More Caregiver-Friendly Practice
1. Clarify HIPAA As Much As Possible
Caregivers often misunderstand HIPAA, and that confusion leads to tension, frustration, and lost opportunities for collaboration. As a provider, you can set the tone early by building simple, repeatable systems to explain what HIPAA actually allows.
Here’s how to clarify HIPAA effectively in your practice:
Normalize the caregiver role: Make it routine to explain that caregivers can share information even without a release. This small clarification goes a long way in building trust.
Offer clear language up front: Add a brief explanation of HIPAA limitations and allowances to your intake forms, follow-up emails, or visit summaries. Keep it in plain, easy-to-follow language.
Train your front desk and clinical staff to respond to common HIPAA questions in a consistent, helpful way.
Use a handout or visual aid to explain HIPAA in simple terms of what can and can’t be shared, and how caregivers can still be involved. Make it available in waiting areas or exam rooms.
Make early consent a standard step. During the first or second visit, offer patients an opportunity to specify what can be shared, and with whom. Keep the conversation low-pressure and collaborative.
Clarity is the key to making sure all parts of the care team are on the same page. When caregivers understand the rules and their role, communication improves.
2. Encourage Proactive Information Sharing
You may not always be able to speak openly with caregivers, but you can always invite them to speak with you. Caregivers often assume they’re not allowed to share anything because of HIPAA. Make it clear that their observations are not only allowed, but valued.
A simple question like “Have you noticed anything new at home?” can open the door. Invite input regularly throughout interactions with caregivers. Acknowledge their role and its unique perspective by saying things like, “You see more than I do—your insight really helps shape treatment.” Finally, make sharing as easy as possible. Offer a secure message line, a dropbox for logs, or a quick paper form for caregivers to fill out at check-in.
Caregivers are often the first to notice changes in mood, medication adherence, or early warning signs. Encouraging them to proactively share that information—even without receiving anything back—improves decision-making, reduces risk, and deepens trust.
3. Work as a Collaborative Partner
Just as caregivers are encouraged to approach providers with a spirit of partnership, providers should do the same. When you approach conversations with a collaborative mindset, it builds trust and improves outcomes.
Use language that reinforces partnership:
“Let’s keep each other updated.”
“We’ll get a clearer picture together.”
Even when you’re limited in what you can share, acknowledging the caregiver’s role and inviting their perspective creates alignment. It also makes it more likely they’ll stay engaged in their loved one’s care plan.
Collaboration doesn’t take extra time. It just takes intention.
4. Have The Consent Talk Early, And Make It Custom
One of the most effective ways to avoid confusion and delays during a crisis is to have clear consent in place from the beginning. When patients are in a more stable state, it’s the ideal time to ask who, if anyone, they’d like to be involved in their care.
A simple, open-ended question like, “Is there anyone you’d want us to loop in for general updates or safety planning?” can start the conversation. From there, offer patients the chance to personalize their consent. Some may want caregivers involved only for medication updates or emergencies, while others may prefer broader communication. Giving them clear, flexible options helps reduce resistance and ensures their preferences are respected.
It’s also important to clarify what HIPAA allows in these conversations, so both patients and caregivers understand the boundaries from the start. Taking time to document these preferences clearly—ideally with a simple form or note in the chart—can prevent last-minute confusion when urgent decisions need to be made.
Early consent isn’t just about legal coverage. It’s about building trust, setting expectations, and keeping everyone aligned in case of any unexpected crises.
5. Share General Resources Without Breaking Privacy Rules
Even when you can’t share personal health details, there’s still a lot you can give caregivers: resources, education, and support that empower them to show up better for their loved one.
Point caregivers toward general educational materials about the condition, recommended treatments, and safety planning. You can also offer guidance on how to communicate more effectively with their loved one or manage stress at home. Support groups, caregiver training programs, and communication skills workshops can all make a meaningful difference, and most don’t require any protected health information to be shared.
Providing these resources takes little time but builds stronger, more informed care teams. It’s a simple way to show caregivers they’re not alone and help reduce the pressure on your practice.
6. Consider Using a Tool That Makes Caregiver Collaboration Easier
The Care Hack was designed to support both caregivers and providers. With a simple referral from their providers, families gain access to expert-led education, coaching, and peer support, with no extra effort required from the clinical team. By equipping caregivers with practical tools and evidence-based guidance, we help them arrive at appointments more informed, more prepared, and more confident. The platform is intentionally low-lift, fitting easily into the workflow of private practices, clinics, and hospitals.
Conclusion: A Better Way Forward
When caregivers and providers collaborate effectively, outcomes improve. Misunderstandings shrink. Crises become more manageable. And trust grows on all sides.
It doesn’t take a system overhaul to get there, just a shared understanding of what’s allowed, what’s helpful, and how to listen. With a little planning and the right tools, we can build a future where no caregiver is left in the dark, and no provider is left to guess what’s happening between visits. At The Care Hack, we’re working to make that future easier to reach, with tools that support caregivers and fit seamlessly into the way providers already work.
Reviewed by Stephanie LeMelle, MD, Chief Clinical Advisor at The Care Hack