3 Major Reasons U.S. Mental Health Care is Failing: A Caregiver’s Guide
3 Major Reasons U.S. Mental Health Care is Failing: A Caregiver’s Guide
Navigating the world of mental health care in the U.S. can often feel like going through a maze without a map. For those helping a loved one with mental illness, it's an uphill battle with seemingly endless challenges. But why?
Why is it so hard to access mental health services in the first place?
And for those who gain access, why is it difficult to find treatments that work?
These questions have bewildered generations of individuals and their families. Indeed, the shortcomings of U.S. mental health represent a reality unbecoming of the world’s wealthiest nation.
Here’s 3 main reasons why today’s health care system falls short of our expectations. (In a following post, we’ll provide tips to help you navigate the system, in spite of these failings.)
3 Major Reasons U.S. Mental Health Care is Failing:
1. The “Show Me The Money” Dilemma: The first reason is simple: not enough money due to a narrow view of costs and return on investment. Insurance companies are inclined to pay for things that will save them money, and most mental health services are not cost saving enough for insurance companies in the short term, even if they have the potential to reduce health care and societal costs long term. This time horizon disconnect often leads insurance companies to provide lower reimbursements for mental health care.
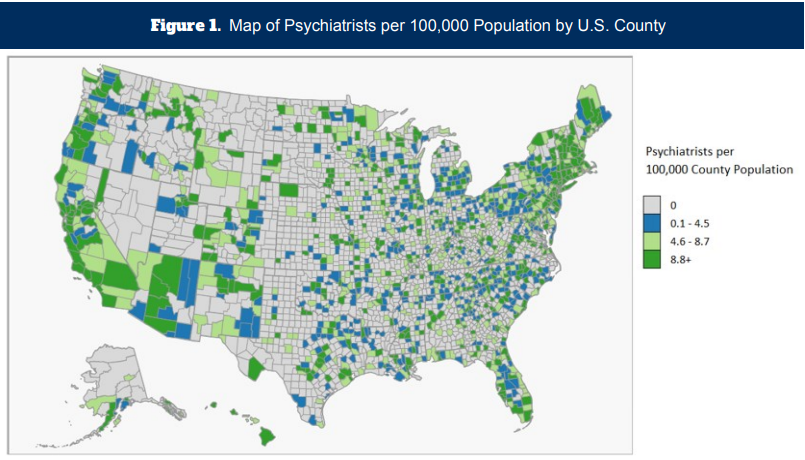
This results in existing providers being discouraged from joining in-network services, and also deters new providers from entering the mental health field, thereby creating a shortage. More than half of U.S. counties lack a single psychiatrist. Of course, people who can afford to pay out of pocket for private services and live in an area with lots of providers, can more easily get access.
But for most Americans, the reality is long wait lists, a lack of in-network providers, and a shortage of open psychiatric hospital beds, which are essential in crisis care. Taken together, these factors add up to a negative impact on care.
Image Source: Behavioral Health Work Force
2. Disconnected Care: The Siloed System Issue. The second big reason the mental health care system falls short is the extreme fragmentation of care. Imagine listening to an orchestra where each instrument is stuck in a different room, playing different music, and can’t hear one another. That's the U.S. mental health care system in a nutshell. This is partially due to privacy and billing rules. HIPAA and other privacy laws make it difficult for professionals to work together as a team, talk to family members, or exchange health records. Patients basically have to start over every time they change providers.
Simultaneously, volume-based billing makes it virtually impossible for providers to spend time collaborating, working on difficult cases, or caring for the sickest patients who need the most help. The need to bill for lots of visits forces providers to see lots of less-sick patients, to make up for the one or two very sick patients that take more time and resources.
As a result, the sickest patients are also those most likely to slip through the cracks. Clinics are not set up with them in mind, since there is no extra reimbursement for the time and resources they consume. Severely ill patients and people in crisis are left with inadequate services, when what they need is the exact opposite: a high quality, integrated approach.
3. Lackluster Results: The third reason U.S. mental health care disappoints, is that standard treatments are simply not as effective as we want them to be. Antidepressants only work for about 60% of people. The science behind antipsychotics for schizophrenia is over 50 years old. In short, we are desperate for new advances in psychiatry. However, even when medications work as intended, especially for people with SMI (Serious Mental Illness), “success” is defined as mere symptom management, i.e. palliative measures.
Rather than aiming for recovery and thriving, we’ve dumbed down the definition of success. For many people with mental illness, medication and therapy is not enough. Individuals with SMI also need “psychosocial support” to have a chance at long-term recovery. Sadly, less than 3% of people with SMI have access to these supports. Being diagnosed with SMI can be a scary, confusing, and demoralizing experience.
It can leave you vulnerable to false hope that a medication, a facility, or a special “consultant” has the answers. Our cofounder Mitul and his family have been there many times caring for his brother. It makes sense that we want to believe our loved ones are treatable, and that the system works. Sadly, the latter is not always true.
Now that you know some of the main reasons our mental health care system falls short, in the next issue we’ll give you some practical tips on how to navigate the system, and get the best possible results, in spite of these failings.
And remember, you don’t have to do it alone! We’re here to support you.
Click here to create a free account and get instant access to expert advice and practical support.